When Gum Disease Meets Diabetes: A Love Story with Too Many Complications
- 4gandroid
- Nov 7, 2024
- 3 min read
Introduction
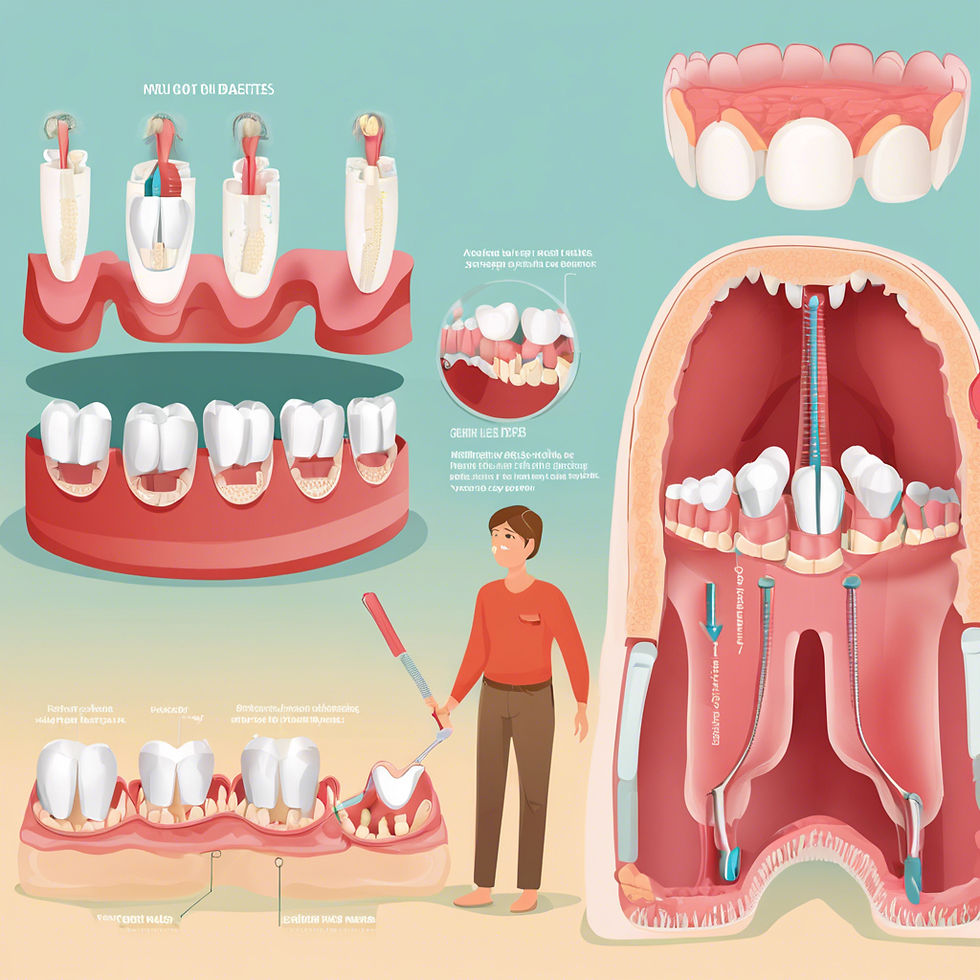
Imagine a world where two silent yet powerful adversaries, gum disease and diabetes, dance together in an intricate exchange of challenges and consequences. Have you ever wondered how these two conditions collide, creating a whirlwind of complications that can jeopardize patient health? What exactly happens when the inflammation of periodontal disease meets the metabolic chaos of diabetes?
For dental professionals entrenched in advanced clinical care, understanding the coexistence of these conditions is paramount. How do cytokines released by gum pathogens influence insulin resistance? In what ways can poor periodontal health hinder glycemic control, creating a cycle of deterioration? As we embark on this exploration, we will uncover the profound implications of this relationship, dissect shared risk factors, and highlight the nuanced management strategies required to help protect our patients from a future fraught with systemic and oral health challenges. Together, let’s delve into this compelling narrative, as we seek answers to these pressing questions in the ongoing battle between gum disease and diabetes—a saga filled with complexities, connections, and ultimately, a quest for healthier outcomes.
The Interconnected Pathophysiology
Diabetes: The Uninvited Guest
Diabetes mellitus, particularly type 2 diabetes, introduces a series of metabolic changes that predispose individuals to periodontal disease. Hyperglycemia can alter neutrophil function, reduce collagen synthesis, and impair wound healing. These physiological alterations create a permissive environment for the proliferation of periodontopathic bacteria.
Immune Dysfunction: Diabetic patients often exhibit a dysregulated immune response characterized by increased levels of inflammatory cytokines and altered chemotaxis of immune cells. This immune dysfunction facilitates the onset and progression of periodontal disease.
Microvascular Complications: The microangiopathy associated with diabetes can diminish blood flow to periodontal tissues, destabilizing the inflammatory response and further contributing to tissue destruction.
Gum Disease: The Cunning Manipulator
Periodontal disease, with its multifactorial etiology rooted in microbial dysbiosis and host inflammatory response, acts as an exacerbator for diabetes. The bacteria involved release lipopolysaccharides (LPS), triggering systemic inflammation and insulin resistance.
Cytokine Cascade: The local inflammation in periodontal tissues can leak systemically, raising levels of pro-inflammatory cytokines such as TNF-α and IL-6, both of which contribute to insulin resistance and poor glycemic control.
LPS and Endotoxemia: The periodontal pocket contains high concentrations of LPS, which can enter the bloodstream, aggravating systemic inflammation and complicating metabolic control.
A Shared Risk Factor: The Porphyromonas gingivalis Connection
At the center of this complicated narrative is Porphyromonas gingivalis, a keystone pathogen in periodontitis linked to increased cardiovascular morbidity and altered glucose metabolism. P. gingivalis can interfere with insulin signaling, further complicating glycemic control in diabetic patients.
Advanced research suggests that the presence of this pathogen could exacerbate complications not just in the oral cavity but systemically, potentially increasing the risk of diabetes-related complications such as nephropathy and retinopathy. This intricate relationship underscores the need for comprehensive health assessments in patients presenting with either condition.
Clinical Management Challenges
Screening and Diagnosis
Early detection is key in managing the entangled relationship between diabetes and gum disease. Clinicians should adopt a comprehensive approach to screening:
Intraoral and Extraoral Assessments: A thorough examination of periodontal health should be routine for all diabetic patients, complemented by systemic screenings for hyperglycemia.
Biomarkers: Research into salivary biomarkers for both periodontal disease and glycemic control holds promise. Advanced practitioners should consider utilizing these as adjunctive diagnostic tools.
Treatment Interventions
The treatment plan must be tailored, addressing both conditions concurrently:
Periodontal Therapy: Utilize a combination of non-surgical periodontal therapy, including scaling and root planing, adjunctive antimicrobials, and possibly local delivery systems of antibiotics in select cases.
Collaborative Care: Work closely with endocrinologists to ensure optimal management of diabetes. A multidisciplinary approach ensures that improvements in glycemic control can facilitate periodontal healing and vice versa.
Patient Education: Empower patients with knowledge about the interplay between their conditions, emphasizing the importance of maintaining good oral hygiene and confirming regular dental visits.
Conclusion
The relationship between gum disease and diabetes is undoubtedly a "love story" fraught with complications that require advanced understanding and management. With a comprehensive and proactive approach, clinicians can navigate this complex nexus, working towards improved outcomes for their patients. By recognizing the shared pathophysiology and engaging in multidisciplinary collaboration, we can turn this tale of woes into a narrative of health restoration, one where the triumph of therapeutic interventions outshines the challenges of intertwined disease processes.
In the end, as with all great love stories, the true victory lies in nurturing a healthier, more vibrant life, a shared journey towards wellness, for our patients and their smiles.




Comments